Some states provide home and community-based behavioral health services for certain Medicaid populations through Section 1915(c) home and community-based services (HCBS) waivers and Section 1915(i) state plan amendments (SPAs). Section 1915(c) waivers and Section 1915(i) SPAs offer states the ability to target services by condition, age, and in the case of Section 1915(c) waivers, geography.
As of September 2015, fourteen states operated a Section 1915(c) waiver for persons with mental illness. Twelve states operated Section 1915(i) SPAs targeting persons with mental illness or substance use disorders. Section 1915(c) waivers and Section 1915(i) SPAs are generally small in size, serving as few as 20 people in a given year.
In total, 18 states offer at least one Section 1915(c) waiver or 1915(i) mental health SPA. Seven states (Connecticut, Indiana, Iowa, Louisiana, Montana, Texas, and Wisconsin) offer both a Section 1915(c) waiver and 1915(i) mental health SPA. States operate fewer 1915(i) SPAs than Section 1915(c) waivers (14 waivers and 12 SPAs, respectively). Section 1915(i) SPAs typically cover fewer services than Section 1915(c) waivers. However, Section 1915(i) SPAs cover more than twice as many enrollees as Section 1915(c) waivers.
States that Operate Section 1915(c) Mental Health Waivers and 1915(i) Mental Health SPAs, as of September 2015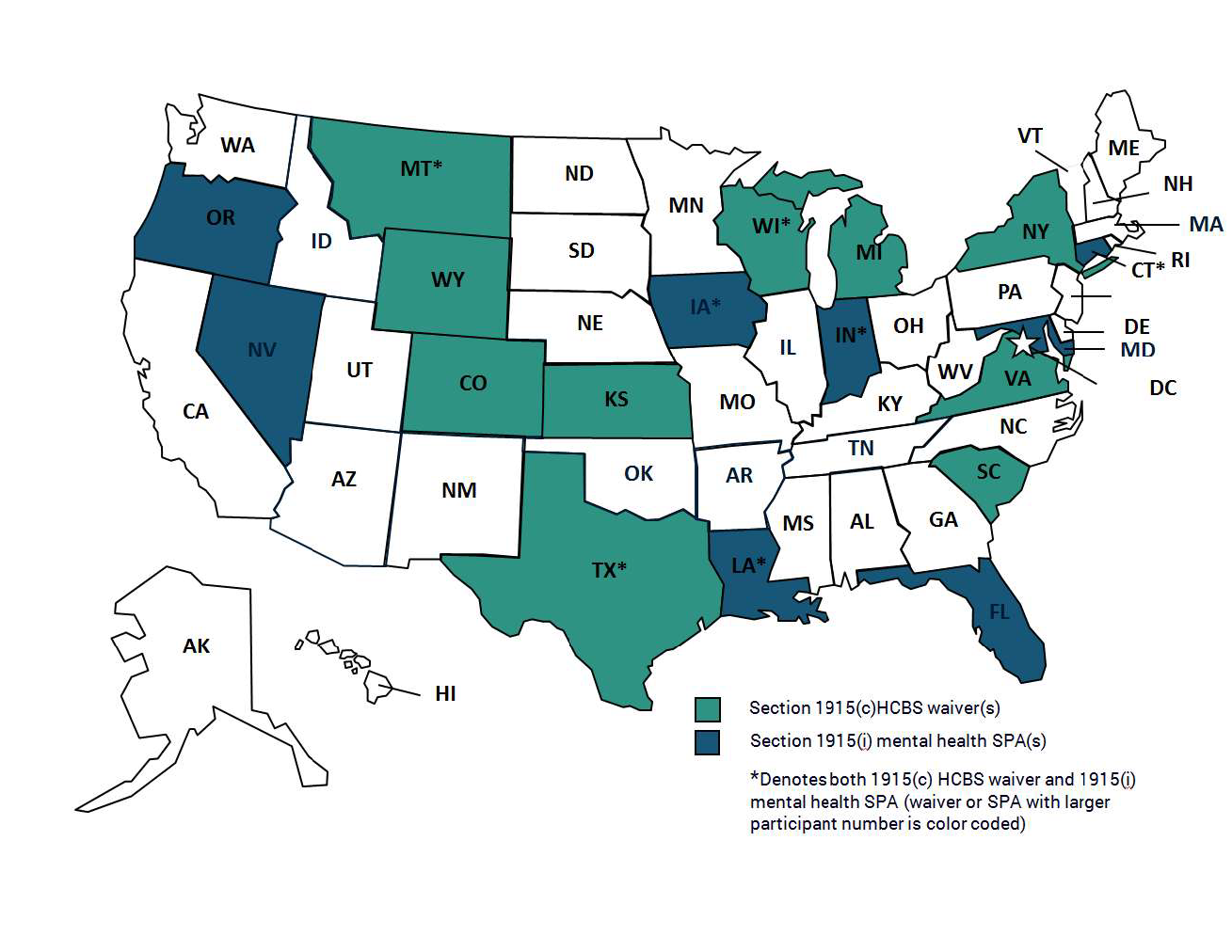
Note: Indiana operates two Section 1915(i) mental health SPAs. Kansas’ waiver expired as of October 1, 2015, but was included in MACPAC’s analysis as it was operational in September 2015.
Source: MACPAC, 2015, analysis of Section 1915(c) of the Social Security Act Medicaid demonstration approvals and Section 1915(i) of the Social Security Act Medicaid state plan amendments.
Section 1915(c) HCBS Waivers
Purpose and use. The Section 1915(c) HCBS waiver was established in 1981 to permit states to offer intensive community-based services comparable to an institutional level of care to people who require long-term services and supports. Such waivers allow states to provide these services to a targeted group of individuals with mental illness, intellectual or developmental disabilities, and physical disabilities. Additionally, a state may provide waiver services to persons with incomes above the Medicaid eligibility level—up to 300 percent of the federal poverty level—who, if not provided HCBS, would require an institutional level of care (42 CFR 435.217).
Number and size. As of September 2015, there were 301 Section 1915(c) demonstration waivers in 47 states and the District of Columbia. Sixteen states used their waivers for mental health services for adults with serious mental illness and children with serious emotional disturbances. Two of the sixteen waivers served only one person and were thus omitted from MACPAC’s analysis of services covered under Section 1915(c) waivers. Five of the waivers offered substance use disorder services.
Two mental health waivers targeted adults, and twelve targeted youth of various ages up to age 21.[1] Six waivers placed a limit on the number of participants enrolled at any one time (Iowa, New York, South Carolina, Texas, Virginia, and Wyoming).
Services. The number and mix of services that states offer under their Section 1915(c) mental health waivers vary by state. The most common service categories were caregiver support; community transition; day services; equipment, technology, and modifications; home-based services; non-medical transportation; other mental health and behavioral; and supported employment (Table 2). Wisconsin is the only state that offered nursing; Connecticut is the only state that offered home-delivered meals; and only Wisconsin and Louisiana offered participant training. No states offered rent and food expenses for live-in caregivers or other health and therapeutic services.[2]
All states offered case management to individuals enrolled in Section 1915(c) waivers consistent with statutory requirements. However, case management services can be delivered either through the waiver or state plan authority. Nine of the fourteen mental health waivers offered some type of case management through the waiver itself (including general case management and wrap-around facilitation).
In addition to case management, several waivers offered multiple services within a service category. Examples of selected services are:
- respite, (11 states);
- home-accessibility adaptation (7 states);
- non-medical transportation (5 states);
- family support and training (5 states); and
- substance use disorder services (4 states).
1915(i) SPA
Purpose and use. The 1915(i) SPA was created in the Deficit Reduction Act of 2005 (DRA, P.L. 109-171) and was updated by the Patient Protection and Affordable Care Act (ACA, P.L. 111-148, as amended) to allow states to provide HCBS services under their Medicaid state plans without obtaining a waiver from CMS (Table 1). Like the Section 1915(c) waiver, the 1915(i) SPA allows states to design service packages targeted to people with specific needs, including special services for those who have developmental disabilities, physical disabilities, mental illness or substance use disorders. States may offer benefits to a specific age group without regard to comparability of services for those who don’t receive the 1915(i) services, although they must abide by the statewideness rule, dictating that state Medicaid programs cannot exclude enrollees or providers because of where they live or work in the state (CMS 2010). Unlike Section 1915(c) waivers, the 1915(i) SPA allows states to set the qualifying level for HCBS at either an institutional level of care or lower.
Number and size. As of September 2015, twelve 1915(i) SPAs served people with mental illness, and seven of them offer at least one substance use service in addition to mental health services. Seven of the SPAs serve adults, four serve children and youth, and one serves all individuals with mental health needs regardless of age.
Services. The most commonly offered service category in 1915(i) mental health SPAs was other mental health and behavioral services, including crisis intervention, behavior support, counseling, and psychosocial rehabilitation. Other commonly offered service categories included caregiver support, case management, day services, home-based services, and supported employment. Several service categories that are statutorily allowed to be offered in 1915(i) SPAs but were not offered by any state include rent and food expenses for live-in caregivers, other health and therapeutic services, and services supporting participant direction. Although federal regulation does not allow for some HCBS services to be offered under state plan authority, the Secretary can approve HCBS services not listed in federal regulation through Section 1915(i) SPAs.
Several 1915(i) mental health SPAs offer more than one service within a service category. Commonly offered services were:
- respite (4 states);
- psychosocial rehabilitation services (4 states);
- peer-to-peer services (4 states); and day habilitation (4 states).
[1] CMS defines Institutions for Mental Disease (IMDs) as inpatient facilities with more than 16 beds that serve populations older than age 21 and younger than age 64 where more than half of the patients are diagnosed with a mental illness (42 USC 1396d).
[2] While state Medicaid programs are not allowed to use federal funds to cover enrollees’ rent and food expenses, federal statute allows states to fund the cost of room and board through Section 1915(c) demonstration waivers for unrelated caregivers providing care to an individual who, without the assistance of a caregiver, would require admission to a hospital, nursing facility, or intermediate care facility for the mentally retarded (§1915(c)(1) of the Act).