Home- and community-based services (HCBS) allow people with significant physical and cognitive limitations to live in their home or a home-like setting and remain integrated with the community. HCBS are optional benefits, and states vary considerably in how they organize their HCBS programs.
- Some states provide certain HCBS in the state plan, which requires that those services be made available to all eligible beneficiaries (although states may include level of care criteria).
- States may also use waiver authorities such as Section 1915(c) HCBS waiver authority, which gives states flexibility to limit the number of beneficiaries receiving services, target specific populations, or limit availability to certain parts of the state. States may also use Section 1115 research and demonstration waivers to provide HCBS, or use some combination of state plan and waiver options.
- The term HCBS encompasses a wide range of services including personal care services provided in a home or residential care setting, supported employment, non-medical transportation, and home-delivered meals. States may not cover the same types of HCBS, or they may cover similar services using different service terms and payment methodologies. Medicaid spending on beneficiaries using HCBS varies widely, particularly for beneficiaries with the greatest long-term services and supports (LTSS) needs (MACPAC 2018).
Medicaid beneficiaries increasingly are receiving LTSS through HCBS. In fiscal year (FY) 2016, Medicaid programs spent approximately $95 billion on HCBS compared to about $67.1 billion on institutional services, which represented a 10 percent increase in HCBS spending over FY 2015 (Murray et al. 2021).
Proportion of Total Medicaid LTSS Spending on Institutional LTSS and HCBS, FYs 2000–2016
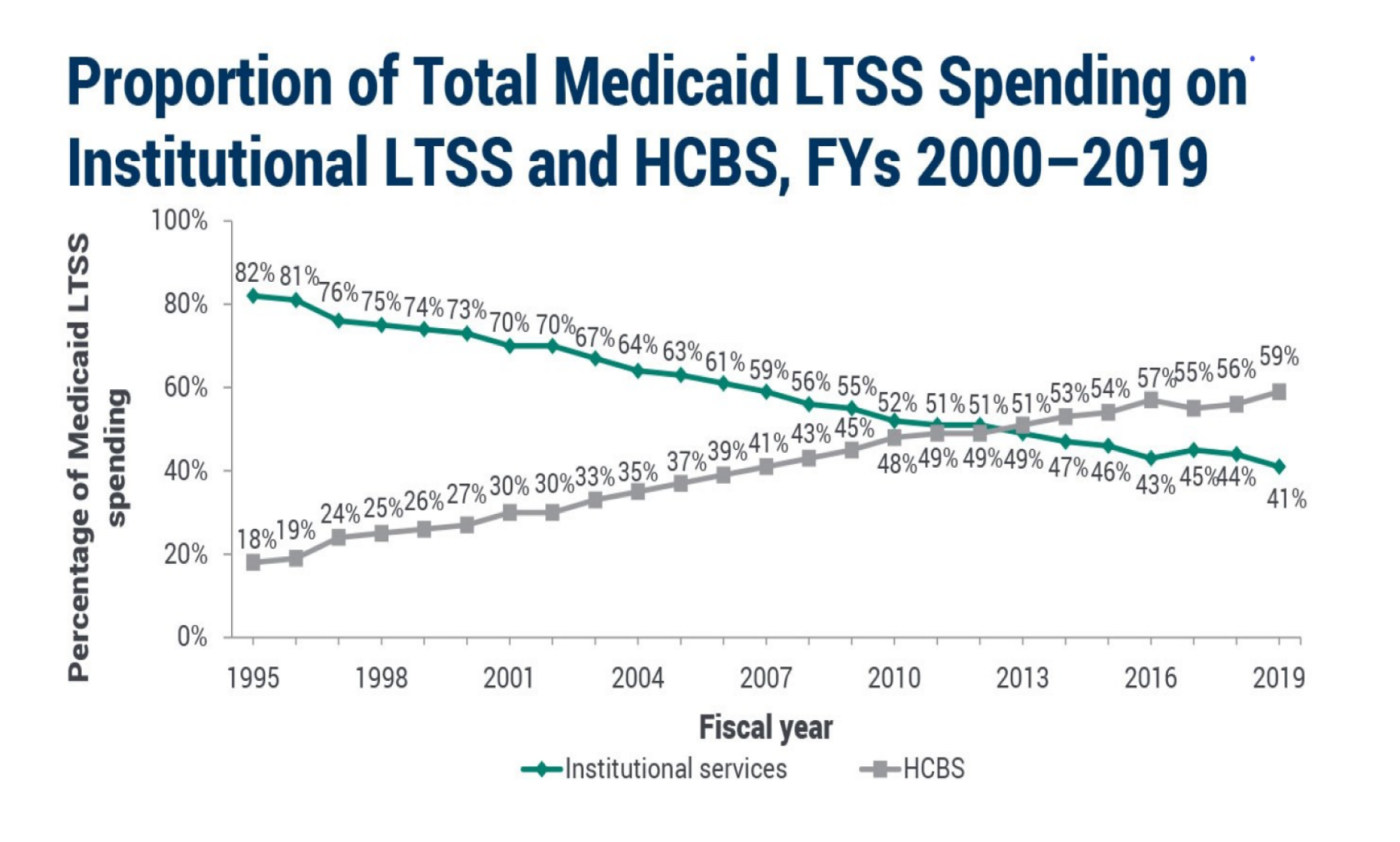
Note: LTSS is long-term services and supports. HCBS is home- and community-based services.
Sources: Eiken, S., K. Sredl, B. Burwell, and R. Woodward 2017 and Eiken, S., K. Sredl, B. Burwell, and A. Amos 2018.
The shift in spending from institutional to home- and community-based settings reflects federal and state policies. Referred to as rebalancing, these efforts have been driven by concerns about the high cost of institutional care and to and meet beneficiary preferences to live in the community. They have included the Money Follows the Person (MFP) demonstration program, which provides participating states with grants to assist beneficiaries living in institutions to transition back to the community. The MFP program was first authorized by the Deficit Reduction Act of 2005 and funding has been extended by subsequent legislation until 2023. States can roll over unused funds for four subsequent four fiscal years. Thus, FY 2023 awards are available through FY 2027.
As HCBS grows as the predominant way of delivering LTSS to Medicaid beneficiaries, HCBS policy continues to evolve. Among current developments in HCBS:
- States are currently implementing new requirements that HCBS settings must meet to be eligible for Medicaid payment. These requirements are meant to ensure that beneficiaries receiving HCBS have adequate choices, their rights are protected, and HCBS is truly integrated into the community. The Centers for Medicare & Medicaid Services are working with states to finalize statewide transition plans to identify providers that do not meet new requirements and to work with them to come into compliance by March 17, 2023. The previous implementation deadline (March 17, 2022) was extended by one year to acknowledge challenges states face during the COVID-19 public health emergency (PHE).
- States also are implementing electronic visit verification (EVV) for personal care services. These commonly are web-based applications that enable personal care services providers to verify their visits to beneficiaries’ residences. EVV helps Medicaid programs ensure that authorized personal care services are delivered. EVV can prevent disruptions in beneficiaries’ care, and protect the Medicaid program against fraud. If a state does not implement EVV by January 1, 2021, its federal funding for personal care services will be reduced.
- A number of efforts are underway to develop and test quality measures for HCBS to aid policymakers in the oversight of LTSS programs. These efforts, which span both Medicaid fee for service and managed LTSS programs, place emphasis on beneficiary experiences and outcomes.
- States take different approaches to managing their HCBS waiver waiting lists, which can influence the length of the waiting list and the wait time before individuals to receive HCBS services.
Learn more
- Compendium: Medicaid Payment Policies for Home- and Community-Based Services in Section 1915(c) Waivers
- State efforts to address Medicaid home-and community-based services workforce shortages
- Examining the potential for additional re-balancing of long-term services and supports
- Medicaid services for people with intellectual or developmental disabilities – evolution of addressing service needs and preferences
- Medicaid home and community-based services: characteristics and spending of high-cost users
- Medicaid payment for services delivered in residential care settings
- Money Follows the Person demonstration program
- Electronic visit verification for personal care services: status of state implementation
- Waiting lists for home- and community-based services